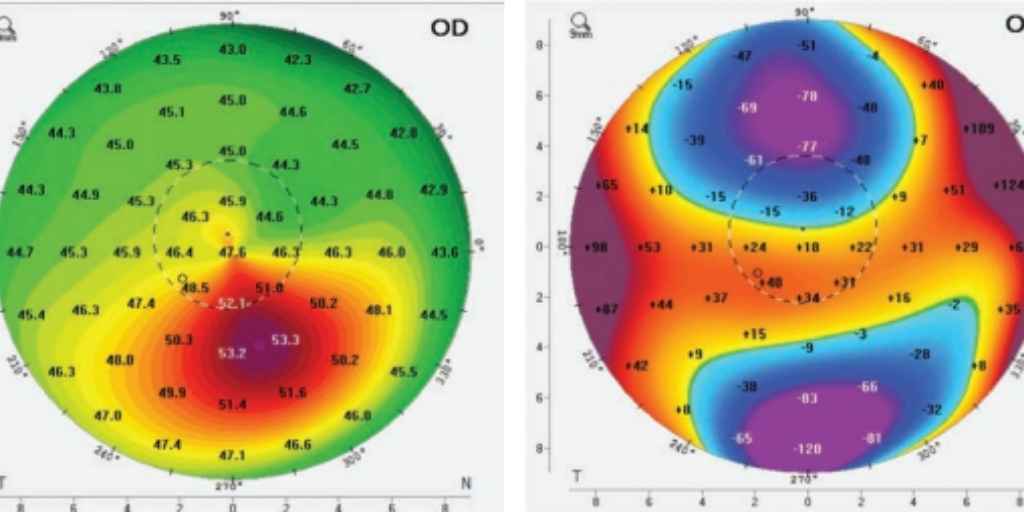
As we discussed in our previous post, Keratoconus is a corneal condition that results in a progressive thinning and bulging of the cornea. This results in irregular astigmatism, which produces blurry or distorted vision. It is typically diagnosed in childhood and progresses into adulthood.
How keratoconus has traditionally been treated?
Initially, glasses or soft, toric contact lenses may correct a person’s vision. As keratoconus progresses, increased distortion and irregular astigmatism is noted. When this occurs, glasses and soft contact lenses no longer adequately correct one’s vision.
When glasses and soft contact lenses don’t provide good vision, the next step is for the patient to be fit with a special medical contact lens. Scleral lenses are a common example of a medical contact lens used to correct a patient’s vision. Scleral lenses are large diameter gas permeable contact lenses that are designed to vault over the cornea and rest on the white part of the eye. By resting on the white part of the eye, these lenses center well on the eye with little to no movement between blinks. These lenses provide a smooth surface to focus the light rays entering the eye.
If scleral contact lenses don’t work for a patient, the next step has traditionally been a full-thickness corneal transplant. In this procedure the central 8-9mm of a patient’s irregular cornea removed and replaced with donor corneal tissue of the same size. This graft tissue is sewn into place. The healing process for this type of surgery can take up to a full year.
What is new in the treatment of keratoconus?
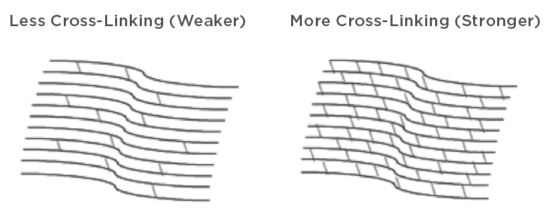
 Corneal collagen cross-linking (CXL) has been a great advancement in the treatment of keratoconus. CXL is a minimally invasive treatment for keratoconus. It is an outpatient procedure that involves applying the combination of riboflavin (vitamin B2) eye drops and ultra-violet A (UVA) light to the eye. The goal of this treatment is to reinforce the collagen fiber links within the cornea. By reinforcing these links, the cornea is both strengthened and stabilized. Corneal collagen cross-linking can slow and possibly halt the progression of keratoconus with the hope of preventing the need of more invasive treatments such as a full-thickness corneal transplant.
Corneal collagen cross-linking (CXL) has been a great advancement in the treatment of keratoconus. CXL is a minimally invasive treatment for keratoconus. It is an outpatient procedure that involves applying the combination of riboflavin (vitamin B2) eye drops and ultra-violet A (UVA) light to the eye. The goal of this treatment is to reinforce the collagen fiber links within the cornea. By reinforcing these links, the cornea is both strengthened and stabilized. Corneal collagen cross-linking can slow and possibly halt the progression of keratoconus with the hope of preventing the need of more invasive treatments such as a full-thickness corneal transplant.
When should I consider cross-linking treatment?
Due to the fact that corneal collagen cross-linking has a quick visual recovery with minimal side effects and can potentially halt the progression of keratoconus, it is worth implementing this treatment at the earliest sign of progression. By treating keratoconus patients with CXL, we can potentially prevent patients who do well with soft toric contact lenses from needing a medically fit scleral lens. We can also potentially prevent those patients who are managed with scleral lenses from progressing to the need for a full-thickness corneal transplant. The earlier we implement treatment with CXL, the better the potential quality of vision for patients.
What should I expect on the day of my cross-linking treatment?
Although the procedure only takes around 1 hour, plan on being at the office for around 2 hours. Numbing drops will be instilled in the eye, making the procedure painless. The cornea is then prepared for the procedure. Riboflavin drops will be applied to the eye. The cornea will be exposed to a UVA light source. At the end of the procedure, a bandage contact lens will be placed on the eye. You will return to the comfort of your home to recover. There is some mild discomfort during the early recovery period. This grittiness and mild burning sensation is typically managed by using artificial tears.
The doctors of Summit Eye Center focus on the diagnosis and treatment of keratoconus. In fact, we have been treating patients with corneal collagen cross-linking for over 5 years. If you have any questions regarding KC or other eye conditions, call us at 816-246-2111 or email